Search
- Page Path
- HOME > Search
- Diabetes, obesity and metabolism
- Triglyceride-Glucose Index Predicts Future Atherosclerotic Cardiovascular Diseases: A 16-Year Follow-up in a Prospective, Community-Dwelling Cohort Study
- Joon Ho Moon, Yongkang Kim, Tae Jung Oh, Jae Hoon Moon, Soo Heon Kwak, Kyong Soo Park, Hak Chul Jang, Sung Hee Choi, Nam H. Cho
- Endocrinol Metab. 2023;38(4):406-417. Published online August 3, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1703

- 2,683 View
- 166 Download
- 3 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
While the triglyceride-glucose (TyG) index is a measure of insulin resistance, its association with cardiovascular disease (CVD) has not been well elucidated. We evaluated the TyG index for prediction of CVDs in a prospective large communitybased cohort.
Methods
Individuals 40 to 70 years old were prospectively followed for a median 15.6 years. The TyG index was calculated as the Ln [fasting triglycerides (mg/dL)×fasting glucose (mg/dL)/2]. CVDs included any acute myocardial infarction, coronary artery disease or cerebrovascular disease. We used a Cox proportional hazards model to estimate CVD risks according to quartiles of the TyG index and plotted the receiver operating characteristics curve for the incident CVD.
Results
Among 8,511 subjects (age 51.9±8.8 years; 47.5% males), 931 (10.9%) had incident CVDs during the follow-up. After adjustment for age, sex, body mass index, diabetes mellitus, hypertension, total cholesterol, smoking, alcohol, exercise, and C-reactive protein, subjects in the highest TyG quartile had 36% increased risk of incident CVD compared with the lowest TyG quartile (hazard ratio, 1.36; 95% confidence interval, 1.10 to 1.68). Carotid plaque, assessed by ultrasonography was more frequent in subjects in the higher quartile of TyG index (P for trend=0.049 in men and P for trend <0.001 in women). The TyG index had a higher predictive power for CVDs than the homeostasis model assessment of insulin resistance (HOMA-IR) (area under the curve, 0.578 for TyG and 0.543 for HOMA-IR). Adding TyG index on diabetes or hypertension alone gave sounder predictability for CVDs.
Conclusion
The TyG index is independently associated with future CVDs in 16 years of follow-up in large, prospective Korean cohort. -
Citations
Citations to this article as recorded by- Construction and validation of a nomogram for predicting diabetes remission at 3 months after bariatric surgery in patients with obesity combined with type 2 diabetes mellitus
Kaisheng Yuan, Bing Wu, Ruiqi Zeng, Fuqing Zhou, Ruixiang Hu, Cunchuan Wang
Diabetes, Obesity and Metabolism.2024; 26(1): 169. CrossRef - Association between the triglyceride glucose index and chronic total coronary occlusion: A cross-sectional study from southwest China
Kaiyong Xiao, Huili Cao, Bin Yang, Zhe Xv, Lian Xiao, Jianping Wang, Shuiqing Ni, Hui Feng, Zhongwei He, Lei Xv, Juan Li, Dongmei Xv
Nutrition, Metabolism and Cardiovascular Diseases.2024; 34(4): 850. CrossRef - The association between TyG and all-cause/non-cardiovascular mortality in general patients with type 2 diabetes mellitus is modified by age: results from the cohort study of NHANES 1999–2018
Younan Yao, Bo Wang, Tian Geng, Jiyan Chen, Wan Chen, Liwen Li
Cardiovascular Diabetology.2024;[Epub] CrossRef - Triglyceride-glucose index predicts type 2 diabetes mellitus more effectively than oral glucose tolerance test-derived insulin sensitivity and secretion markers
Min Jin Lee, Ji Hyun Bae, Ah Reum Khang, Dongwon Yi, Mi Sook Yun, Yang Ho Kang
Diabetes Research and Clinical Practice.2024; 210: 111640. CrossRef - Evaluation of the novel three lipid indices for predicting five- and ten-year incidence of cardiovascular disease: findings from Kerman coronary artery disease risk factors study (KERCADRS)
Alireza Jafari, Hamid Najafipour, Mitra Shadkam, Sina Aminizadeh
Lipids in Health and Disease.2023;[Epub] CrossRef
- Construction and validation of a nomogram for predicting diabetes remission at 3 months after bariatric surgery in patients with obesity combined with type 2 diabetes mellitus

- Diabetes, Obesity and Metabolism
- Incretin and Pancreatic β-Cell Function in Patients with Type 2 Diabetes
- Chang Ho Ahn, Tae Jung Oh, Se Hee Min, Young Min Cho
- Endocrinol Metab. 2023;38(1):1-9. Published online February 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.103
- 3,335 View
- 362 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
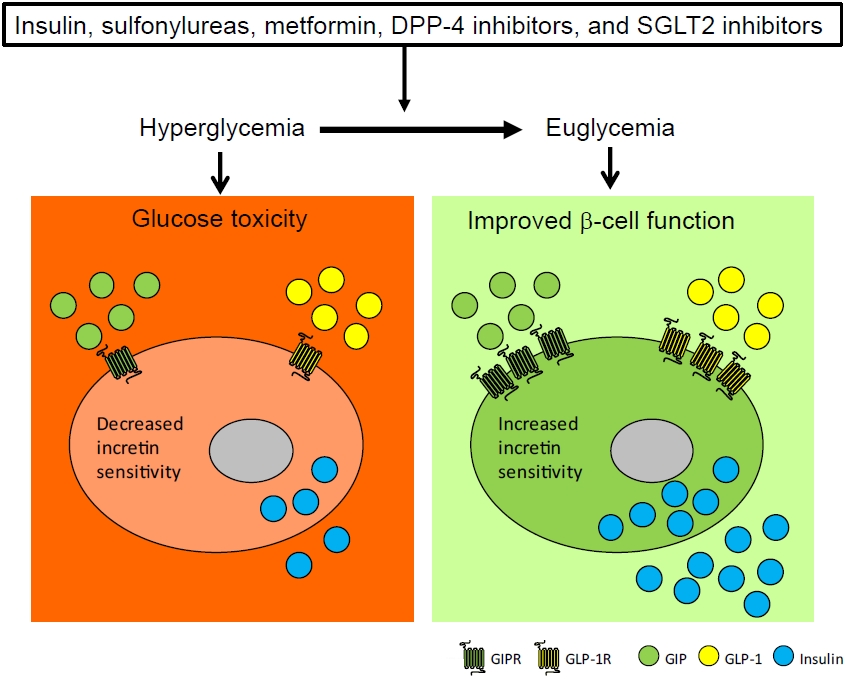
ePub - To maintain normal glucose homeostasis after a meal, it is essential to secrete an adequate amount of insulin from pancreatic β-cells. However, if pancreatic β-cells solely depended on the blood glucose level for insulin secretion, a surge in blood glucose levels would be inevitable after the ingestion of a large amount of carbohydrates. To avoid a deluge of glucose in the bloodstream after a large carbohydrate- rich meal, enteroendocrine cells detect the amount of nutrient absorption from the gut lumen and secrete incretin hormones at scale. Since insulin secretion in response to incretin hormones occurs only in a hyperglycemic milieu, pancreatic β-cells can secrete a “Goldilocks” amount of insulin (i.e., not too much and not too little) to keep the blood glucose level in the normal range. In this regard, pancreatic β-cell sensitivity to glucose and incretin hormones is crucial for maintaining normal glucose homeostasis. In this Namgok lecture 2022, we review the effects of current anti-diabetic medications on pancreatic β-cell sensitivity to glucose and incretin hormones.
-
Citations
Citations to this article as recorded by- Initial Combination Therapy in Type 2 Diabetes
Ji Yoon Kim, Nam Hoon Kim
Endocrinology and Metabolism.2024; 39(1): 23. CrossRef
- Initial Combination Therapy in Type 2 Diabetes

- Diabetes, Obesity and Metabolism
- The Presence of Clonal Hematopoiesis Is Negatively Associated with Diabetic Peripheral Neuropathy in Type 2 Diabetes
- Tae Jung Oh, Han Song, Youngil Koh, Sung Hee Choi
- Endocrinol Metab. 2022;37(2):243-248. Published online April 25, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1337
- 3,351 View
- 123 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
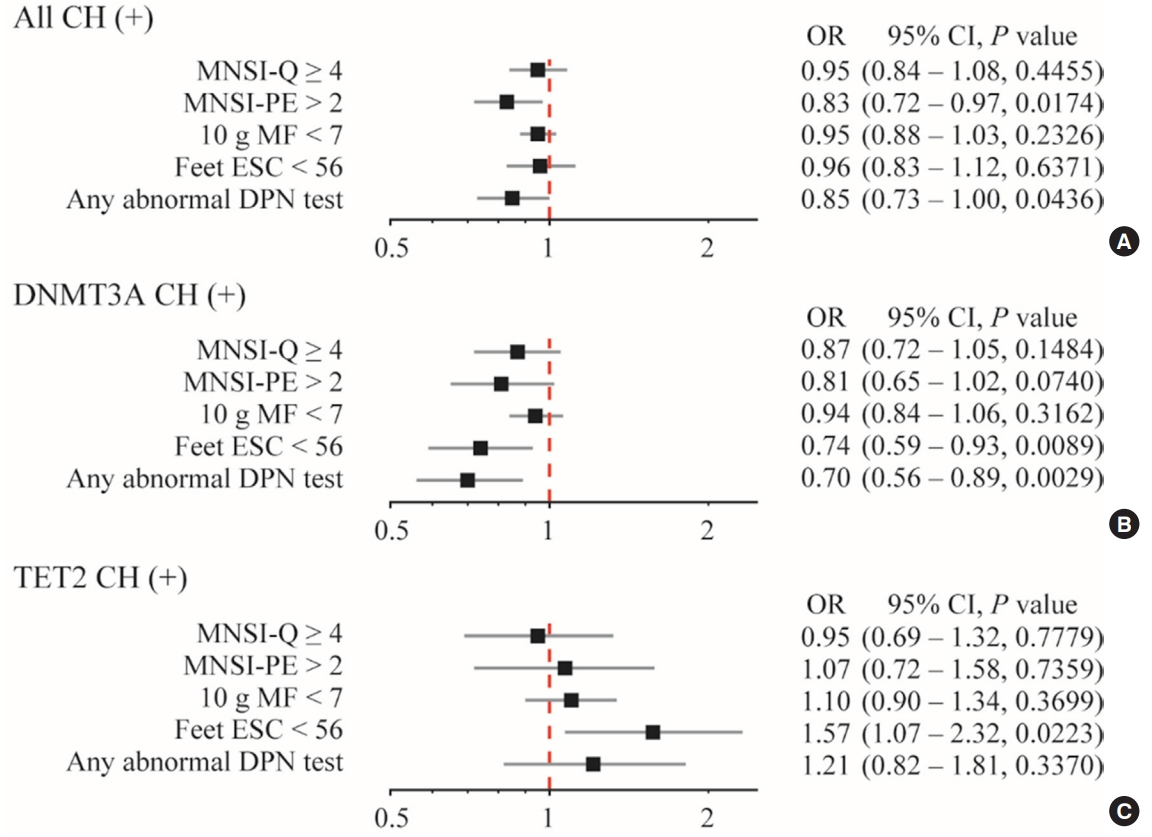
Clonal hematopoiesis of indeterminate potential (CHIP) has been reported to be associated with increased cardiovascular disease, aging and insulin resistance. Despite the debate of causal contribution of CHIP on metabolic diseases, we want to explore whether CHIP is related to diabetic peripheral neuropathy (DPN).
Methods
This study analyzed the prevalence of CHIP in patients with type 2 diabetes classified according to DPN status. Logistic regression analysis was used to evaluate the association between CHIP and DPN.
Results
CHIP was more prevalent in subjects without DPN than those with DPN (19.9% vs. 8.8%, respectively; P=0.013). Individuals having any CHIP, or DNA methyltransferase 3A (DNMT3A) CHIP were less likely to have any abnormality shown in DPN test; the adjusted odds ratio were 0.85 (95% confidence interval [CI], 0.73 to 1.00) and 0.70 (95% CI, 0.56 to 0.89), respectively. Interestingly, DNMT3A CHIP showed the negative association, but Tet methylcytosine dioxygenase 2 (TET2) CHIP showed the positive association with abnormal feet electrochemical skin conductance level.
Conclusion
On the contrary to expectations, CHIP was negatively associated with DPN. Functional linking between the mutation in hematopoietic cells and DPN, and the opposite role of DNMT3A and TET2 should be investigated. -
Citations
Citations to this article as recorded by- TET2 mutation as prototypic clonal hematopoiesis lesion
Luca Guarnera, Babal K. Jha
Seminars in Hematology.2024; 61(1): 51. CrossRef - Clonal hematopoiesis with DNMT3A mutation is associated with lower white matter hyperintensity volume
Woo‐Jin Lee, Keun‐Hwa Jung, Han Song, Heesun Lee, Hyo Eun Park, Youngil Koh, Su‐Yeon Choi, Kyung‐Il Park
CNS Neuroscience & Therapeutics.2023; 29(5): 1243. CrossRef
- TET2 mutation as prototypic clonal hematopoiesis lesion

- Clinical Study
- Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes
- Han Na Jang, Ye Seul Yang, Seong Ok Lee, Tae Jung Oh, Bo Kyung Koo, Hye Seung Jung
- Endocrinol Metab. 2019;34(4):382-389. Published online December 23, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.4.382
- 4,996 View
- 143 Download
- 7 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Conflicting results have been reported on the efficacy of insulin degludec/insulin aspart (IDegAsp) compared to basal insulin in type 2 diabetes. We investigated the effects of changing basal insulin to IDegAsp on glycemic control and sought to identify factors related to those effects.
Methods In this retrospective study of patients from three referral hospitals, patients with type 2 diabetes using basal insulin with hemoglobin A1c (HbA1c) levels less than 11.0% were enrolled. Basal insulin was replaced with IDegAsp, and data were analyzed from 3 months before to 3 months after the replacement.
Results Eighty patients were recruited (52.5% male; mean age, 67.0±9.8 years; mean duration of diabetes, 18.9±8.5 years; mean HbA1c, 8.7%±1.0%). HbA1c levels increased during 3 months of basal insulin use, but significantly decreased after changing to IDegAsp (8.28%±1.10%,
P =0.0001). The reduction was significant at 6 months in 35 patients whose longer-term data were available. Patients with a measured fasting plasma glucose (m-FPG) lower than their predicted FPG (p-FPG) by regression from HbA1c showed a significant HbA1c reduction caused by the change to IDegAsp, even without a significantly increased insulin dose. However, patients whose m-FPG was higher than their p-FPG did not experience a significant HbA1c reduction, despite a significantly increased insulin dose. Furthermore, the HbA1c reduction caused by IDegAsp was significant in patients with low fasting C-peptide levels and high insulin doses.Conclusion We observed a significant glucose-lowering effect by replacing basal insulin with IDegAsp, especially in patients with a lower m-FPG than p-FPG.
-
Citations
Citations to this article as recorded by- Evaluation of the efficiency of insulin degludec/insulin aspart therapy in controlling hyperglycemia and hypoglycemia in patients with type 2 diabetes mellitus: a real-life experience
Gökçen Güngör Semiz, İsmail Selimoğlu, Mehmet Emin Arayici, Serkan Yener, Abdurrahman Çömlekçi, Tevfik Demir
International Journal of Diabetes in Developing Countries.2023; 43(4): 544. CrossRef - Low fasting glucose‐to‐estimated average glucose ratio was associated with superior response to insulin degludec/aspart compared with basal insulin in patients with type 2 diabetes
Han Na Jang, Ye Seul Yang, Tae Jung Oh, Bo Kyung Koo, Seong Ok Lee, Kyong Soo Park, Hak Chul Jang, Hye Seung Jung
Journal of Diabetes Investigation.2022; 13(1): 85. CrossRef - Efficacy and Safety of Insulin Degludec/Insulin Aspart (IDegAsp) in Type 2 Diabetes: Systematic Review and Meta-Analysis
Brenda C Edina, Jeremy R Tandaju, Lowilius Wiyono
Cureus.2022;[Epub] CrossRef - Comparing time to intensification between insulin degludec/insulin aspart and insulin glargine: A single-center experience from India
Rajiv Kovil
Journal of Diabetology.2022; 13(2): 171. CrossRef - Efficacy and Safety of Insulin Degludec/Insulin Aspart Compared with a Conventional Premixed Insulin or Basal Insulin: A Meta-Analysis
Shinje Moon, Hye-Soo Chung, Yoon-Jung Kim, Jae-Myung Yu, Woo-Ju Jeong, Jiwon Park, Chang-Myung Oh
Metabolites.2021; 11(9): 639. CrossRef - Fear of Hypoglycemia in Adults with diabetes mellitus switching to Treatment with IDegAsp Co-formulation to Examine real-world setting: an observational study (The HATICE study)
Ulaş Serkan Topaloğlu, Hatice Kayış Topaloğlu, Melih Kızıltepe, Mesut Kılıç, Sami Bahçebaşı, Sibel Ata, Şeyma Yıldız, Yasin Şimşek
Drug Metabolism and Drug Interactions.2021; 36(2): 129. CrossRef - Response: Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes (Endocrinol Metab 2019; 34:382-9, Han Na Jang et al.)
Han Na Jang, Hye Seung Jung
Endocrinology and Metabolism.2020; 35(1): 194. CrossRef - Letter: Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes (Endocrinol Metab 2019; 34:382-9, Han Na Jang et al.)
Sang Youl Rhee
Endocrinology and Metabolism.2020; 35(1): 192. CrossRef - Fear of hypoglycemia in adults with diabetes mellitus switching to treatment with IDegAsp co-formulation to examine real-world setting: an observational study (The HATICE study)
Ulaş Serkan Topaloğlu, Hatice Kayış Topaloğlu, Melih Kızıltepe, Mesut Kılıç, Sami Bahçebaşı, Sibel Ata, Şeyma Yıldız, Yasin Şimşek
Drug Metabolism and Personalized Therapy.2020;[Epub] CrossRef
- Evaluation of the efficiency of insulin degludec/insulin aspart therapy in controlling hyperglycemia and hypoglycemia in patients with type 2 diabetes mellitus: a real-life experience

- Thyroid
- Validity and Reliability of the Korean Version of the Hyperthyroidism Symptom Scale
- Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
- Endocrinol Metab. 2018;33(1):70-78. Published online March 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.1.70
- 4,051 View
- 55 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Thyrotoxicosis is a common disease resulting from an excess of thyroid hormones, which affects many organ systems. The clinical symptoms and signs are relatively nonspecific and can vary depending on age, sex, comorbidities, and the duration and cause of the disease. Several symptom rating scales have been developed in an attempt to assess these symptoms objectively and have been applied to diagnosis or to evaluation of the response to treatment. The aim of this study was to assess the reliability and validity of the Korean version of the hyperthyroidism symptom scale (K-HSS).
Methods Twenty-eight thyrotoxic patients and 10 healthy subjects completed the K-HSS at baseline and after follow-up at Seoul National University Bundang Hospital. The correlation between K-HSS scores and thyroid function was analyzed. K-HSS scores were compared between baseline and follow-up in patient and control groups. Cronbach's α coefficient was calculated to demonstrate the internal consistency of K-HSS.
Results The mean age of the participants was 34.7±9.8 years and 13 (34.2%) were men. K-HSS scores demonstrated a significant positive correlation with serum free thyroxine concentration and decreased significantly with improved thyroid function. K-HSS scores were highest in subclinically thyrotoxic subjects, lower in patients who were euthyroid after treatment, and lowest in the control group at follow-up, but these differences were not significant. Cronbach's α coefficient for the K-HSS was 0.86.
Conclusion The K-HSS is a reliable and valid instrument for evaluating symptoms of thyrotoxicosis in Korean patients.
-
Citations
Citations to this article as recorded by- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Effect of increased levothyroxine dose on depressive mood in older adults undergoing thyroid hormone replacement therapy
Jae Hoon Moon, Ji Won Han, Tae Jung Oh, Sung Hee Choi, Soo Lim, Ki Woong Kim, Hak Chul Jang
Clinical Endocrinology.2020; 93(2): 196. CrossRef - Clinical Feasibility of Monitoring Resting Heart Rate Using a Wearable Activity Tracker in Patients With Thyrotoxicosis: Prospective Longitudinal Observational Study
Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
JMIR mHealth and uHealth.2018; 6(7): e159. CrossRef
- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)

- Endocrine Research
- Effects of Lobeglitazone, a New Thiazolidinedione, on Osteoblastogenesis and Bone Mineral Density in Mice
- Kyoung Min Kim, Hyun-Jin Jin, Seo Yeon Lee, Hyo Jin Maeng, Gha Young Lee, Tae Jung Oh, Sung Hee Choi, Hak Chul Jang, Soo Lim
- Endocrinol Metab. 2017;32(3):389-395. Published online September 18, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.3.389
- 4,770 View
- 51 Download
- 11 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Bone strength is impaired in patients with type 2 diabetes mellitus despite an increase in bone mineral density (BMD). Thiazolidinedione (TZD), a peroxisome proliferator activated receptor γ agonist, promotes adipogenesis, and suppresses osteoblastogenesis. Therefore, its use is associated with an increased risk of fracture. The aim of this study was to examine the
in vitro andin vivo effects of lobeglitazone, a new TZD, on bone.Methods MC3T3E1 and C3H10T1/2 cells were cultured in osteogenic medium and exposed to lobeglitazone (0.1 or 1 µM), rosiglitazone (0.4 µM), or pioglitazone (1 µM) for 10 to 14 days. Alkaline phosphatase (ALP) activity, Alizarin red staining, and osteoblast marker gene expression were analyzed. For
in vivo experiments, 6-month-old C57BL/6 mice were treated with vehicle, one of two doses of lobeglitazone, rosiglitazone, or pioglitazone. BMD was assessed using a PIXImus2 instrument at the baseline and after 12 weeks of treatment.Results As expected,
in vitro experiments showed that ALP activity was suppressed and the mRNA expression of osteoblast marker genes RUNX2 (runt-related transcription factor 2) and osteocalcin was significantly attenuated after rosiglitazone treatment. By contrast, lobeglitazone at either dose did not inhibit these variables. Rosiglitazone-treated mice showed significantly accelerated bone loss for the whole bone and femur, but BMD did not differ significantly between the lobeglitazone-treated and vehicle-treated mice.Conclusion These findings suggest that lobeglitazone has no detrimental effects on osteoblast biology and might not induce side effects in the skeletal system.
-
Citations
Citations to this article as recorded by- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Y
Diabetes & Metabolism Journal.2022; 46(6): 855. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Lobeglitazone: A Novel Thiazolidinedione for the Management of Type 2 Diabetes Mellitus
Jaehyun Bae, Taegyun Park, Hyeyoung Kim, Minyoung Lee, Bong-Soo Cha
Diabetes & Metabolism Journal.2021; 45(3): 326. CrossRef - Effect of lobeglitazone on motor function in rat model of Parkinson’s disease with diabetes co-morbidity
Kambiz Hassanzadeh, Arman Rahimmi, Mohammad Raman Moloudi, Rita Maccarone, Massimo Corbo, Esmael Izadpanah, Marco Feligioni
Brain Research Bulletin.2021; 173: 184. CrossRef - Comparison of the Effects of Various Antidiabetic Medication on Bone Mineral Density in Patients with Type 2 Diabetes Mellitus
Jeonghoon Ha, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Seung Hyun Ko, Moo Il Kang, Sung Dae Moon, Ki-Hyun Baek
Endocrinology and Metabolism.2021; 36(4): 895. CrossRef - Xenogeneic native decellularized matrix carrying PPARγ activator RSG regulating macrophage polarization to promote ligament-to-bone regeneration
Xue Han, Lijun Liao, Tian Zhu, Yuchan Xu, Fei Bi, Li Xie, Hui Li, Fangjun Huo, Weidong Tian, Weihua Guo
Materials Science and Engineering: C.2020; 116: 111224. CrossRef - Diabetes pharmacotherapy and effects on the musculoskeletal system
Evangelia Kalaitzoglou, John L. Fowlkes, Iuliana Popescu, Kathryn M. Thrailkill
Diabetes/Metabolism Research and Reviews.2019;[Epub] CrossRef - The effects of diabetes therapy on bone: A clinical perspective
Karim G. Kheniser, Carmen M. Polanco Santos, Sangeeta R. Kashyap
Journal of Diabetes and its Complications.2018; 32(7): 713. CrossRef
- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis

- Adrenal gland
- In Vivo Models for Incretin Research: From the Intestine to the Whole Body
- Tae Jung Oh
- Endocrinol Metab. 2016;31(1):45-51. Published online March 16, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.1.45
- 4,041 View
- 52 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Incretin hormones are produced by enteroendocrine cells (EECs) in the intestine in response to ingested nutrient stimuli. The incretin effect is defined as the difference in the insulin secretory response between the oral glucose tolerance test and an isoglycemic intravenous glucose infusion study. The pathophysiology of the decreased incretin effect has been studied as decreased incretin sensitivity and/or β-cell dysfunction
per se . Interestingly, robust increases in endogenous incretin secretion have been observed in many types of metabolic/bariatric surgery. Therefore, metabolic/bariatric surgery has been extensively studied for incretin physiology, not only the hormones themselves but also alterations in EECs distribution and genetic expression levels of gut hormones. These efforts have given us an enormous understanding of incretin biology from synthesis toin vivo behavior. Further innovative studies are needed to determine the mechanisms and targets of incretin hormones.-
Citations
Citations to this article as recorded by- High-intensity infrasound effects on glucose metabolism in rats
Gonçalo Martins Pereira, Madalena Santos, Sofia S. Pereira, Gonçalo Borrecho, Francisco Tortosa, José Brito, Diamantino Freitas, António Oliveira de Carvalho, Artur Águas, Maria João Oliveira, Pedro Oliveira
Scientific Reports.2021;[Epub] CrossRef - Parboiled rice metabolism differs in healthy and diabetic individuals with similar improvement in glycemic response
Samar Hamad, Tasleem A. Zafar, Jiwan Sidhu
Nutrition.2018; 47: 43. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Fibroblast growth factor 21 is required for beneficial effects of exercise during chronic high-fat feeding
Christine Loyd, I. Jack Magrisso, Michael Haas, Sowmya Balusu, Radha Krishna, Nobuyuki Itoh, Darleen A. Sandoval, Diego Perez-Tilve, Silvana Obici, Kirk M. Habegger
Journal of Applied Physiology.2016; 121(3): 687. CrossRef
- High-intensity infrasound effects on glucose metabolism in rats

- Obesity and Metabolism
- Glucagon-Like Peptide-1 Increases Mitochondrial Biogenesis and Function in INS-1 Rat Insulinoma Cells
- Mi Yeon Kang, Tae Jung Oh, Young Min Cho
- Endocrinol Metab. 2015;30(2):216-220. Published online June 30, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.2.216
- 4,014 View
- 44 Download
- 41 Web of Science
- 40 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Glucagon-like peptide-1 (GLP-1) is a gut-derived incretin hormone that increases glucose-stimulated insulin secretion in pancreatic β-cells. Since mitochondrial function is crucial to insulin secretion, we hypothesized that GLP-1 may increase mitochondrial biogenesis in pancreatic β-cells. We treated INS-1 rat insulinoma cells with GLP-1 or exendin-4 for 48 hours and measured mitochondrial mass and function. Both GLP-1 and exendin-4 increased mitochondrial mass by approximately 20%. The mitochondria/cytosol ratio was increased from 7.60±3.12% to 10.53±2.70% by exendin-4. In addition, GLP-1 increased the mitochondrial membrane potential and oxygen consumption. Proliferator-activated receptor-gamma coactivator 1α expression was increased approximately 2-fold by GLP-1 treatment. In conclusion, the present study presents evidence for a new mechanism of action by which GLP-1 improves pancreatic β-cell function via enhanced mitochondrial mass and performance.
-
Citations
Citations to this article as recorded by- New fraternine analogues: Evaluation of the antiparkinsonian effect in the model of Parkinson's disease
Andréia Biolchi Mayer, Henrique de Oliveira Amaral, Danilo Gustavo R. de Oliveira, Gabriel Avohay Alves Campos, Priscilla Galante Ribeiro, Solange Cristina Rego Fernandes, Adolfo Carlos Barros de Souza, Raffael Júnio Araújo de Castro, Anamélia Lorenzetti
Neuropeptides.2024; 103: 102390. CrossRef - Prospects of antidiabetic drugs in the treatment of neurodegenerative disease
Lidan Hu, Wenmin Wang, Xiangjun Chen, Guannan Bai, Liangjian Ma, Xin Yang, Qiang Shu, Xuekun Li
Brain‐X.2024;[Epub] CrossRef - Attenuating mitochondrial dysfunction and morphological disruption with PT320 delays dopamine degeneration in MitoPark mice
Vicki Wang, Kuan-Yin Tseng, Tung-Tai Kuo, Eagle Yi-Kung Huang, Kuo-Lun Lan, Zi-Rong Chen, Kuo-Hsing Ma, Nigel H. Greig, Jin Jung, Ho-II Choi, Lars Olson, Barry J. Hoffer, Yuan-Hao Chen
Journal of Biomedical Science.2024;[Epub] CrossRef - Liraglutide demonstrates a therapeutic effect on mitochondrial dysfunction in human SGBS adipocytes in vitro
Maija Vaittinen, Mariana Ilha, Elena Herbers, Anita Wagner, Kirsi A. Virtanen, Kirsi H. Pietiläinen, Eija Pirinen, Jussi Pihlajamäki
Diabetes Research and Clinical Practice.2023; 199: 110635. CrossRef - The cardioprotective effect of human glucagon‐like peptide‐1 receptor agonist (semaglutide) on cisplatin‐induced cardiotoxicity in rats: Targeting mitochondrial functions, dynamics, biogenesis, and redox status pathways
Marwa Mohamed Atef, Yasser Mostafa Hafez, Omnia Safwat El‐Deeb, Eman H. Basha, Radwa Ismail, Hanan Alshenawy, Rasha Osama El‐Esawy, Amira Kamel Eltokhy
Cell Biochemistry and Function.2023; 41(4): 450. CrossRef - Targeting mitochondrial quality control for diabetic cardiomyopathy: Therapeutic potential of hypoglycemic drugs
Yutong Zhou, Wendong Suo, Xinai Zhang, Jiaojiao Liang, Weizhe Zhao, Yue Wang, Hong Li, Qing Ni
Biomedicine & Pharmacotherapy.2023; 168: 115669. CrossRef - Soft X-ray tomography to map and quantify organelle interactions at the mesoscale
Valentina Loconte, Jitin Singla, Angdi Li, Jian-Hua Chen, Axel Ekman, Gerry McDermott, Andrej Sali, Mark Le Gros, Kate L. White, Carolyn A. Larabell
Structure.2022; 30(4): 510. CrossRef - Comparisons of pleiotropic effects of SGLT2 inhibition and GLP-1 agonism on cardiac glucose intolerance in heart dysfunction
Belma Turan, Aysegul Durak, Yusuf Olgar, Erkan Tuncay
Molecular and Cellular Biochemistry.2022; 477(11): 2609. CrossRef - Modulation of Reactive Oxygen Species Homeostasis as a Pleiotropic Effect of Commonly Used Drugs
Carolin Thomas, Lia Wurzer, Ernst Malle, Michael Ristow, Corina T. Madreiter-Sokolowski
Frontiers in Aging.2022;[Epub] CrossRef - Anti-cancer effects of sitagliptin, vildagliptin, and exendin-4 on triple-negative breast cancer cells via mitochondrial modulation
POOJA JAISWAL, VERSHA TRIPATHI, ANSHUL ASSAIYA, DHARMENDRA KASHYAP, RAHUL DUBEY, ANAMIKA SINGH, JANESH KUMAR, HEM CHANDRA JHA, RAJESH SHARMA, AMIT KUMAR DIXIT, HAMENDRA SINGH PARMAR
BIOCELL.2022; 46(12): 2645. CrossRef - Effect of liraglutide on neural and peripheral markers of metabolic function during antipsychotic treatment in rats
Ilijana Babic, Dominic Sellers, Paul L Else, Jessica Nealon, Ashleigh L Osborne, Nagesh Pai, Katrina Weston-Green
Journal of Psychopharmacology.2021; 35(3): 284. CrossRef - Sustained Release GLP-1 Agonist PT320 Delays Disease Progression in a Mouse Model of Parkinson’s Disease
Vicki Wang, Tung-Tai Kuo, Eagle Yi-Kung Huang, Kuo-Hsing Ma, Yu-Ching Chou, Zhao-Yang Fu, Li-Wen Lai, Jin Jung, Hoi-II Choi, Doo-Sup Choi, Yazhou Li, Lars Olson, Nigel H. Greig, Barry J. Hoffer, Yuan-Hao Chen
ACS Pharmacology & Translational Science.2021; 4(2): 858. CrossRef - Antioxidative Potentials of Incretin-Based Medications: A Review of Molecular Mechanisms
Habib Yaribeygi, Mina Maleki, Thozhukat Sathyapalan, Tannaz Jamialahmadi, Amirhossein Sahebkar, Marina Sokovi
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - Vernicia fordii (Hemsl.) Airy Shaw extract stimulates insulin secretion in pancreatic β-cells and improves insulin sensitivity in diabetic mice
Jimin Hyun, Mi Hyeon Park, Yo Han Lee, Youngeun Lee, Su Ji Jeong, Sun Sil Choi, Keon Woo Khim, Hye Jin Eom, Jin-Hoe Hur, Chan Young Park, Jae-Ick Kim, Jiyoung Park, Hyung Won Ryu, Hyun-Jun Jang, Sei-Ryang Oh, Jang Hyun Choi
Journal of Ethnopharmacology.2021; 278: 114238. CrossRef - Connecting the dots between mitochondrial dysfunction and Parkinson’s disorder: focus mitochondria-targeting therapeutic paradigm in mitigating the disease severity
Ishnoor Kaur, Tapan Behl, Aayush Sehgal, Sukhbir Singh, Neelam Sharma, Lotfi Aleya, Simona Bungau
Environmental Science and Pollution Research.2021; 28(28): 37060. CrossRef - Neuromodulatory effects of anti-diabetes medications: A mechanistic review
Habib Yaribeygi, Milad Ashrafizadeh, Neil C. Henney, Thozhukat Sathyapalan, Tannaz Jamialahmadi, Amirhossein Sahebkar
Pharmacological Research.2020; 152: 104611. CrossRef - Antidiabetic Agents for Treatment of Parkinson’s Disease: A Meta-Analysis
Shu-Yi Wang, Shey-Lin Wu, Ta-Cheng Chen, Chieh-Sen Chuang
International Journal of Environmental Research and Public Health.2020; 17(13): 4805. CrossRef - Visualizing subcellular rearrangements in intact β cells using soft x-ray tomography
Kate L. White, Jitin Singla, Valentina Loconte, Jian-Hua Chen, Axel Ekman, Liping Sun, Xianjun Zhang, John Paul Francis, Angdi Li, Wen Lin, Kaylee Tseng, Gerry McDermott, Frank Alber, Andrej Sali, Carolyn Larabell, Raymond C. Stevens
Science Advances.2020;[Epub] CrossRef - Nutrient Sensor mTOR and OGT: Orchestrators of Organelle Homeostasis in Pancreatic β-Cells
Nicholas Esch, Seokwon Jo, Mackenzie Moore, Emilyn U. Alejandro, Yingke Xu
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Metabolic dynamics of human Sertoli cells are differentially modulated by physiological and pharmacological concentrations of GLP-1
Ana D. Martins, Mariana P. Monteiro, Branca M. Silva, Alberto Barros, Mário Sousa, Rui A. Carvalho, Pedro F. Oliveira, Marco G. Alves
Toxicology and Applied Pharmacology.2019; 362: 1. CrossRef - Sarcopenia in Chronic Kidney Disease: Factors, Mechanisms, and Therapeutic Interventions
Hiroshi Watanabe, Yuki Enoki, Toru Maruyama
Biological and Pharmaceutical Bulletin.2019; 42(9): 1437. CrossRef - Recent Advances in Drug Repurposing for Parkinson’s Disease
Xin Chen, Giuseppe Gumina, Kristopher G. Virga
Current Medicinal Chemistry.2019; 26(28): 5340. CrossRef - Mitochondrial dysfunction in diabetes and the regulatory roles of antidiabetic agents on the mitochondrial function
Habib Yaribeygi, Stephen L. Atkin, Amirhossein Sahebkar
Journal of Cellular Physiology.2019; 234(6): 8402. CrossRef - Liraglutide protects against glucolipotoxicity‐induced RIN‐m5F β‐cell apoptosis through restoration of PDX1 expression
Edy Kornelius, Hsin‐Hua Li, Chiung‐Huei Peng, Yi‐Sun Yang, Wei‐Jen Chen, Yan‐Zin Chang, Yi‐Chiao Bai, Stanley Liu, Chien‐Ning Huang, Chih‐Li Lin
Journal of Cellular and Molecular Medicine.2019; 23(1): 619. CrossRef - The osteogenic effect of liraglutide involves enhanced mitochondrial biogenesis in osteoblasts
Subhashis Pal, Shailendra K. Maurya, Sourav Chattopadhyay, Shyamsundar Pal China, Konica Porwal, Chirag Kulkarni, Sabyasachi Sanyal, Rohit A. Sinha, Naibedya Chattopadhyay
Biochemical Pharmacology.2019; 164: 34. CrossRef - Novel Treatment Opportunities Against Cognitive Impairment in Parkinson’s Disease with an Emphasis on Diabetes-Related Pathways
Holly Green, Panagiota Tsitsi, Ioanna Markaki, Dag Aarsland, Per Svenningsson
CNS Drugs.2019; 33(2): 143. CrossRef - Mitral cells and the glucagon‐like peptide 1 receptor: The sweet smell of success?
Enrico Bagnoli, Una FitzGerald
European Journal of Neuroscience.2019; 49(4): 422. CrossRef - Targeting the DPP-4-GLP-1 pathway improves exercise tolerance in heart failure patients: a systematic review and meta-analysis
Chengcong Chen, Ying Huang, Yongmei Zeng, Xiyan Lu, Guoqing Dong
BMC Cardiovascular Disorders.2019;[Epub] CrossRef - Acute exposure to 3‑deoxyglucosone at high glucose levels impairs insulin secretion from β‑cells by downregulating the sweet taste receptor signaling pathway
Xiudao Song, Guoqiang Liang, Min Shi, Liang Zhou, Fei Wang, Lurong Zhang, Fei Huang, Guorong Jiang
Molecular Medicine Reports.2019;[Epub] CrossRef - Translational approaches to restoring mitochondrial function in Parkinson's disease
Heather Mortiboys, Ruby Macdonald, Thomas Payne, Matilde Sassani, Thomas Jenkins, Oliver Bandmann
FEBS Letters.2018; 592(5): 776. CrossRef - Neuroprotective exendin-4 enhances hypothermia therapy in a model of hypoxic-ischaemic encephalopathy
Eridan Rocha-Ferreira, Laura Poupon, Aura Zelco, Anna-Lena Leverin, Syam Nair, Andrea Jonsdotter, Ylva Carlsson, Claire Thornton, Henrik Hagberg, Ahad A Rahim
Brain.2018; 141(10): 2925. CrossRef - Current perspective of mitochondrial biology in Parkinson's disease
Navneet Ammal Kaidery, Bobby Thomas
Neurochemistry International.2018; 117: 91. CrossRef - Humanin promotes mitochondrial biogenesis in pancreatic MIN6 β-cells
Qingqing Qin, Jieqiong Jin, Fang He, Yongqin Zheng, Tingting Li, Yun Zhang, Jundong He
Biochemical and Biophysical Research Communications.2018; 497(1): 292. CrossRef - Exenatide once weekly versus placebo in Parkinson's disease: a randomised, double-blind, placebo-controlled trial
Dilan Athauda, Kate Maclagan, Simon S Skene, Martha Bajwa-Joseph, Dawn Letchford, Kashfia Chowdhury, Steve Hibbert, Natalia Budnik, Luca Zampedri, John Dickson, Yazhou Li, Iciar Aviles-Olmos, Thomas T Warner, Patricia Limousin, Andrew J Lees, Nigel H Grei
The Lancet.2017; 390(10103): 1664. CrossRef - Alogliptin, a Dipeptidyl Peptidase‐4 Inhibitor, Alleviates Atrial Remodeling and Improves Mitochondrial Function and Biogenesis in Diabetic Rabbits
Xiaowei Zhang, Zhiwei Zhang, Yungang Zhao, Ning Jiang, Jiuchun Qiu, Yajuan Yang, Jian Li, Xue Liang, Xinghua Wang, Gary Tse, Guangping Li, Tong Liu
Journal of the American Heart Association.2017;[Epub] CrossRef - Potential therapeutic interventions for chronic kidney disease‐associated sarcopenia via indoxyl sulfate‐induced mitochondrial dysfunction
Yuki Enoki, Hiroshi Watanabe, Riho Arake, Rui Fujimura, Kana Ishiodori, Tadashi Imafuku, Kento Nishida, Ryusei Sugimoto, Saori Nagao, Shigeyuki Miyamura, Yu Ishima, Motoko Tanaka, Kazutaka Matsushita, Hirotaka Komaba, Masafumi Fukagawa, Masaki Otagiri, To
Journal of Cachexia, Sarcopenia and Muscle.2017; 8(5): 735. CrossRef - The pancreas: Bandmaster of glucose homeostasis
Nathalie Jouvet, Jennifer L. Estall
Experimental Cell Research.2017; 360(1): 19. CrossRef - The glucagon-like peptide 1 (GLP) receptor as a therapeutic target in Parkinson's disease: mechanisms of action
Dilan Athauda, Thomas Foltynie
Drug Discovery Today.2016; 21(5): 802. CrossRef - Effects of addition of a dipeptidyl peptidase IV inhibitor to metformin on sirolimus-induced diabetes mellitus
Long Jin, Sun Woo Lim, Jian Jin, Byung Ha Chung, Chul Woo Yang
Translational Research.2016; 174: 122. CrossRef - Pharmacological Modulators of Endoplasmic Reticulum Stress in Metabolic Diseases
Tae Jung, Kyung Choi
International Journal of Molecular Sciences.2016; 17(2): 192. CrossRef
- New fraternine analogues: Evaluation of the antiparkinsonian effect in the model of Parkinson's disease

- Characterization of Incidentally Detected Adrenal Pheochromocytoma.
- Ye An Kim, Yul Hwangbo, Min Joo Kim, Hyung Jin Choi, Je Hyun Seo, Yenna Lee, Soo Heun Kwak, Eu Jeong Ku, Tae Jung Oh, Eun Roh, Jae Hyun Bae, Jung Hee Kim, Kyoung Soo Park, Seong Yeon Kim
- Endocrinol Metab. 2012;27(2):132-137. Published online June 20, 2012
- DOI: https://doi.org/10.3803/EnM.2012.27.2.132
- 2,289 View
- 28 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
In approach to an adrenal incidentaloma, early exclusion of pheochromocytoma is clinically important, due to the risk of catecholamine crisis. The aims of this study are to investigate the characteristics of incidentally detected pheochromocytomas, compared with that of the other adrenal incidentalomas, and to compare these characteristics with those of symptomatic pheochromocytomas. METHODS: In this retrospective study, we reviewed the medical records of 198 patients with adrenal incidentaloma from 2001 to 2010. We analyzed the clinical, laboratory and radiological data of pheochromocytomas, in comparison with those of the other adrenal incidentalomas. We also compared the characteristics of these incidentally detected pheochromocytomas with the medical records of 28 pathologically proven pheochromocytomas, diagnosed based on typical symptoms. RESULTS: Among the 198 patients with adrenal incidentaloma, nineteen patients were diagnosed with pheochromocytoma. Pheochromocytomas showed larger size and higher Hounsfield unit at precontrast computed tomography (CT) than did non-pheochromocytomas. All pheochromocytomas were larger than 2.0 cm, and the Hounsfield units were 19 or higher in precontrast CT. When both criteria of size > 2.0 cm and Hounsfield unit > 19 were met, the sensitivity and specificity for the diagnosis of pheochromocytoma were 100% and 79.3%, respectively. Compared with patients with pheochromocytoma, diagnosed based on typical symptoms, patients with incidentally detected pheochromocytoma were older, presented less often with hypertension, and showed lower levels of 24-hour urine metanephrine. CONCLUSION: Adrenal incidentaloma with < 2.0 cm in size or < or = 19 Hounsfield units in precontrast CT imaging was less likely to be a pheochromocytoma. Patients with incidentally discovered pheochromocytoma showed lower catecholamine metabolites, compared with those patients with symptomatic pheochromocytoma. -
Citations
Citations to this article as recorded by- Guidelines for the Management of Adrenal Incidentaloma: the Korean Endocrine Society, Committee of Clinical Practice Guidelines
Jung-Min Lee, Mee Kyoung Kim, Seung-Hyun Ko, Jung-Min Koh, Bo-Yeon Kim, Sang-Wan Kim, Soo-Kyung Kim, Hae-Jin Kim, Ohk-Hyun Ryu, Juri Park, Jung-Soo Lim, Seong Yeon Kim, Young Kee Shong, Soon Jib Yoo
The Korean Journal of Medicine.2017; 92(1): 4. CrossRef - Clinical Guidelines for the Management of Adrenal Incidentaloma
Jung-Min Lee, Mee Kyoung Kim, Seung-Hyun Ko, Jung-Min Koh, Bo-Yeon Kim, Sang Wan Kim, Soo-Kyung Kim, Hae Jin Kim, Ohk-Hyun Ryu, Juri Park, Jung Soo Lim, Seong Yeon Kim, Young Kee Shong, Soon Jib Yoo
Endocrinology and Metabolism.2017; 32(2): 200. CrossRef - Characterization of Incidentally Detected Adrenal Pheochromocytoma
Soon Jib Yoo, Woohyeon Kim
Endocrinology and Metabolism.2012; 27(2): 116. CrossRef
- Guidelines for the Management of Adrenal Incidentaloma: the Korean Endocrine Society, Committee of Clinical Practice Guidelines


 KES
KES

 First
First Prev
Prev



